2018 marked the 100th anniversary of the Spanish Flu (H1N1) pandemic. CDC statistics from the 1918 pandemic show that approximately 500 million people  worldwide were infected. That was one-third of the world’s population at the time! The number of deaths was estimated to be at least 50 million across the globe, including about 675,000 in the U.S.
worldwide were infected. That was one-third of the world’s population at the time! The number of deaths was estimated to be at least 50 million across the globe, including about 675,000 in the U.S.
According to the World Health Organization, the next pandemic is most likely to be caused by influenza. What does this mean for physicians and patients, and what can all of us to do prepare?
What Defines a Pandemic?
Before we go any further, let’s assume that not everyone understands the difference between an epidemic and a pandemic. Merriam-Webster defines a pandemic as an outbreak of a disease that occurs over a wide geographic area and affects an exceptionally high proportion of the population. The outbreak is typically sudden and the mortality rate is high. In contrast, an epidemic is a widespread occurrence of a disease in a community at a particular time.
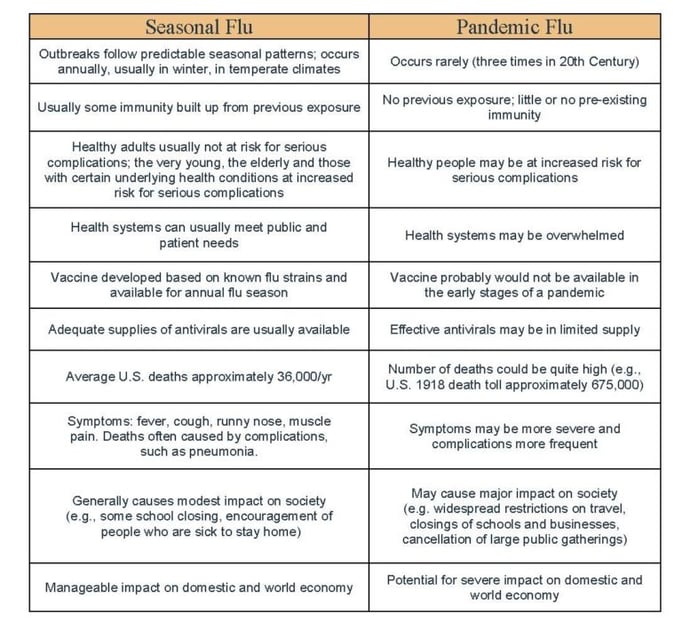
The typical flu season is what the CDC defines as seasonal flu, which happens annually without added complications such as overwhelmed medical providers and an effective vaccine. Pandemic flu and season flu have some significant differences:
But We Aren’t Living a Disaster Movie…Right?
What are the chances of another flu pandemic? Ask the next person you meet on the street, and they might believe it’s nearly impossible. Actually, most of us have already lived through the swine flu, in 2009. There were also pandemics in the 1970s, 1960s, and 1950s. The only thing that remains constant about influenza is that the virus is constantly changing, and thus requires continued surveillance and vigilance to protect the world not only from seasonal influenza but also from novel influenza A viruses that could trigger a pandemic.
A, B, C, or D?
No, it’s not a multiple-choice question—it’s the four types of influenza viruses. Human influenza A and B viruses cause seasonal epidemics of disease. When a new and different influenza A virus emerges, its infection rate can cause an influenza pandemic. Type C infections generally cause a mild respiratory illness, and type D viruses do not affect humans.
These new viruses are what concern the healthcare community at large. It’s likely that “H7N9” isn’t yet on your radar, but perhaps it should be. No, H7N9 isn’t the newest droid in the latest Star Wars movie—human infections with this Asian lineage avian influenza A virus were first reported in China in March 2013. While there have only been three reported human infections since October 2017, and the CDC does not have any special recommendations regarding this strain, it does have pandemic potential. It is possible for this strain to mutate and gain the ability to spread easily and sustainably among people. The CDC states that of the novel influenza A viruses that are of special concern to public health, Asian lineage H7N9 virus is rated by the Influenza Risk Assessment Tool as having the greatest potential to cause a pandemic.
How To Prepare
If another flu pandemic is inevitable (and it is), how should the healthcare community at large and the general public prepare? It’s vital that we prepare—scientists estimate that if the 1918 flu pandemic happened today, the death toll could be as high as 147million.
Recent years have also seen expanded global and domestic surveillance. The CDC is using sequencing technology to detect emerging novel or reassortant viruses, inform vaccine strain selection, and detect and monitor antiviral resistance.
On the consumer end, a misunderstanding of how the flu vaccine works and how important it is to get one, especially for children and the elderly, persists. All those that are involved (manufacturers, the CDC, healthcare providers, etc) must continue to help consumers understand the importance of the vaccine and why they should get one even if it doesn’t always work.
If we don’t continue to push—push for better flu vaccines, push for better therapies, push for better diagnostics, push to make sure facilities have processes and procedures in place to respond to a pandemic, and push to make sure kids and the elderly are vaccinated—only then will we truly be unprepared for the next pandemic.
Manufacturers continue to work on accurate diagnostic tests that pick up all flu strains. Recently, rapid antigen influenza diagnostics were re-classified by the FDA as Class II devices with Special Controls. Regulated as Class I, they did not all meet the needs of patients, physicians, or public health, resulting in misdiagnosis and increased mortality. The Class I devices have since been removed from the market.
Sekisui Diagnostics offers the OSOM® Ultra Flu A&B Test, an in vitro rapid qualitative test that detects influenza type A and type B nucleoprotein antigens directly from nasal swab,



Share Article