
Stroke is the third leading cause of disability worldwide.1 The proportion of people with disability five years after stroke ranges from 25% among those who had minor strokes to about 50% among those who had moderate strokes and 80% among those who had severe strokes. Ten years after a stroke, roughly half of survivors are disabled.
Survivors of stroke often experience2:
- Paralysis, weakness, or both on one side of the body.
- Trouble with thinking, awareness, attention, learning, judgment and memory.
- Problems understanding or forming speech.
- Trouble controlling or expressing emotions.
- Numbness or strange sensations.
- Pain in the hands and feet that worsens with movement and temperature changes.
- Trouble with chewing and swallowing.
- Problems with bladder and bowel control.
- Depression.
Pragmatic solutions to reduce the burden of stroke and related diseases are urgently needed to save lives and improve brain health, quality of life and global socioeconomic productivity.
Pragmatic solutions to reduce the burden of stroke and related diseases are urgently needed to save lives and improve brain health
Barriers to Effective Rehabilitation
Effective rehabilitation services call for an experienced multidisciplinary team (including physicians, speech therapists, physiotherapists, occupational therapists, nurses, prosthetists, orthotists, and other healthcare professionals trained in stroke rehabilitation); an individualized, goal-oriented approach; and appropriate equipment and facilities.4 But many barriers stand in the way of this gold standard.
For example, poor service organization and a lack of protocols for rehabilitation have led to prolonged waiting times for the assessment of individual needs, hospital discharges without a rehabilitation plan, inadequate long-term support, inadequate screening and care for depression, and little psychological and social support.5
In addition, the complexity of rehabilitation services and the multitude of settings in which they may be delivered (e.g., inpatient care, outpatient care, community care and home care) create barriers in terms of securing funding, governing the workforce and services, capturing and reporting data, and quality improvement and care coordination.6
Another barrier is the fact that stroke rehabilitation is often focused only on a narrow range of services, for a limited time, and in only some settings.7 For example:
- Only physiotherapy may be available, with little access to other specialties, such as speech therapy, occupational therapy and neuropsychology.
- Publicly funded rehabilitation services may be provided in acute-care settings, but not in the community, in patients’ homes or via telemedicine.
- Access to the broadest scope of services may be reserved for patients in large cities with the ability to pay privately.
What’s more, a broad range of stakeholders lack much awareness of the role of rehabilitation after stroke, resulting in low political will to fund services and little advocacy to increase access to them.8
Equally apparent are gaps in which practice recommendations are not supported by evidence, including recommendations for complex interdisciplinary rehabilitation for patients with prolonged disorders of consciousness, optimal speech therapy for patients with aphasia (i.e., the loss of the ability to understand or express speech) and treatment of neurovisual disorders.9 Gaps in evidence also exist for treatment of post-stroke fatigue and cognitive, emotional and behavioral disorders.
One study shows that even though speech-language pathologists frequently use counselling to support psychological well-being in people with post-stroke aphasia (a patient group particularly vulnerable to mood disorders), they report low knowledge, skill and confidence in the practice.10
New Approaches to Stroke Rehabilitation
Researchers and practitioners continue to explore new approaches to stroke rehabilitation. Some are quite low-tech.
For example, studies have demonstrated that dance may facilitate changes in balance and fall risk, encourage confidence, promote comfort with the changed body, increase rehabilitation motivation, and facilitate community reintegration.11
In some lower-income countries, responsibility for stroke rehabilitation has been taken up by individuals who propagate services and run training programs.12 Online, internationally led mentoring programs have been found to prevent the so-called brain drain of health professionals who must emigrate to get training in stroke rehabilitation, but who fail to return to their country of origin to apply their skills.
High-tech solutions are being explored as well. Even though the application of artificial intelligence is lagging in stroke rehabilitation, studying the gait kinematics (i.e., the factors affecting the ability to walk or run) of individuals with stroke may provide information for deep-learning models to predict the results of clinical assessments and exercise recommendations made by physiotherapists.13
Neuromuscular electrical stimulation (NMES) is another promising intervention, but more rigorous studies are needed to determine its effectiveness.14 Researchers continue to gather evidence on other interventions associated with stroke rehabilitation, including robotic therapy, aquatic therapy, and virtual reality and video gaming.
A recent technological solution is vagus nerve stimulation to treat upper extremity motor deficits associated with chronic ischemic stroke (i.e., stroke caused by a blockage of blood flow to the brain).15 The system electrically stimulates the vagus nerve—a nerve that runs from the brain down to the abdomen—to improve patients’ ability to move their arms and hands.
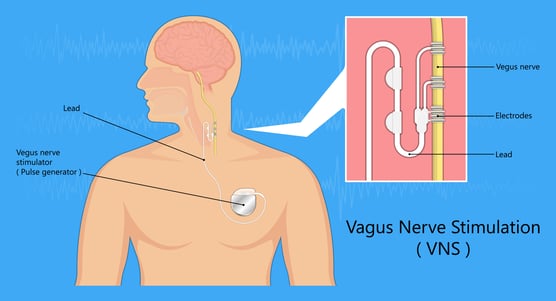 Illustration of Vagus Nerve Stimulation
Illustration of Vagus Nerve Stimulation
Many patients poststroke may wonder if there is anything they can do at home to improve their motor outcomes. Though evidence is scant about the effectiveness of home-based therapy programs to improve arm recovery, recent reviews suggest that virtual reality, robotics and interactive video gaming hold great promise for movement-based therapies at home.16
The Heart & Stroke Foundation of Canada has compiled a checklist for patients, families and caregivers to enable self-management following stroke, including monitoring movement (move more, sit less), eating well and safely (sit upright), and exercising arms, legs, sense of touch, vision, attention and memory.17 Recovery is a process that can last months and even years, the Foundation points out. People with stroke must challenge their bodies – safely -- every day, and keep in mind that everyone’s recovery is different.
References
- Pragmatic solutions to reduce the global burden of stroke: a World Stroke Organization–Lancet Neurology Commission, The Lancet Neurology, page 1
- Treat and Recover from Stroke, Centers for Disease Control and Prevention
- Pragmatic solutions to reduce the global burden of stroke: a World Stroke Organization–Lancet Neurology Commission, The Lancet Neurology, page 1
- Ibid, page 30
- Ibid, page 31
- Ibid
- Ibid
- Ibid
- Ibid, page 32
- Counselling education for speech-language pathology students in Australia: a survey of education in post-stroke aphasia, Taylor & Francis Online
- Dance interventions for individuals post-stroke - a scoping review, Taylor & Francis Online
- Pragmatic solutions to reduce the global burden of stroke: a World Stroke Organization–Lancet Neurology Commission, The Lancet Neurology, page 31
- Development of a convolutional neural network (CNN) based assessment exercise recommendation system for individuals with chronic stroke: a feasibility study, Taylor & Francis Online
- Interventions to Improve Movement and Functional Outcomes in Adult Stroke Rehabilitation: Review and Evidence Summary, Journal of Participatory Medicine
- FDA Approves First-of-Its-Kind Stroke Rehabilitation System, U.S. Food and Drug Administration
- Interventions to Improve Movement and Functional Outcomes in Adult Stroke Rehabilitation: Review and Evidence Summary, Journal of Participatory Medicine
- Enabling self-management following stroke: A checklist for patients, families, and caregivers, Heart and Stroke Foundation of Canada


Share Article