Molecular diagnostics (MDx) is the rapidly developing area of laboratory medicine that investigates human, viral and microbial genomes and the products they encode. Molecular diagnostic techniques and platforms are playing a larger and more critical role in all areas of anatomic and clinical pathology. In the last decade or so, the clinical laboratory has seen an explosion in the available menu of tests based upon DNA and RNA analysis. The completion of the Human Genome Project and the rapid advancement of technology to arise out
 of that effort has moved from the research bench to the clinical laboratory bench with swift success. For the first time in the history of the diagnostic laboratory, molecular pathology and diagnostics are extending the range of information available to physicians, pharmacists, geneticists, forensic scientists, research scientists and other healthcare professionals.
of that effort has moved from the research bench to the clinical laboratory bench with swift success. For the first time in the history of the diagnostic laboratory, molecular pathology and diagnostics are extending the range of information available to physicians, pharmacists, geneticists, forensic scientists, research scientists and other healthcare professionals.
Timeline Examples of Molecular Diagnostics
While the ongoing SARS-CoV-2 / COVID-19 pandemic helped make molecular terms like ‘polymerase chain reaction’ (PCR), ‘false positive’ and ‘variant’ common, the field actually dates to 1949 with Linus Pauling and colleagues’ characterization of sickle cell anemia as a ‘molecular disease.’ However, it took decades for the scientific discipline of molecular biology to develop and become usable in the medical laboratory as a basis for disease diagnostics. MDx grew from the early days of recombinant DNA technology. Sequencing and cDNA cloning were critical for establishing basic knowledge on the primary sequence of various genes. DNA probes incorporating radioactive nucleotides allowed the analysis, via Southern blotting, of genomic regions, leading to the concept and application of restriction fragment length polymorphism (RFLP) to track variant alleles in the human genome.
In 1976, Kan et al. were the first to make a prenatal diagnosis of α-thalassemia using MDx techniques. This diagnostic, alongside the use of RFLP to characterize sickle cell alleles, set the foundation for characterization of other genetic diseases (e.g., cystic fibrosis), as well as infectious diseases, using MDx platforms.
The development of PCR in the mid 1980s led to the golden era of molecular biology and MDx, and the use of a thermostable DNA polymerase from Thermus aquaticus (i.e., Taq polymerase, Saiki et al., 1988) quickly ushered this technique into the realm of laboratory medicine. With its powerful ability to exponentially amplify a target sequence, PCR allows the identification of a known mutation or sequence within hours.
Not only did PCR bolster MDx in the clinical laboratory, it provided a foundation for the design and development of many variant detection schemes based on the amplification of DNA. It helped establish 3 categories for variant detection, depending on the basis for discriminating the allelic variants:
- enzymatic-based methods
- electrophoretic-based methods
- solid phase-based methods
While many of these methods are now infrequently used in clinical microbiology, they paved the way to current, more sophisticated methods.
Molecular Diagnostics Challenges
Twenty-six years ago, the U.S. Food and Drug Administration approved the first direct-specimen molecular testing for infectious diseases. Since that time, the rapid advancement of molecular technology has been driven by 2 primary areas: automated extraction, amplification and detection platforms and next-generation sequencing.
As with any new advanced area, there are challenges and limitations that the laboratory medicine and public health fields must pay close attention to as these developments intersect with the care of patients and healthcare and public health policy.
The cost of this advanced technology could lead to further health disparities if economic decisions limit the use of MDx to certain communities or populations. Another challenge of advanced and rapidly implemented MDx platforms is potential over- or underutilization. For example, rapid MDx platforms are often faster and more sensitive than traditional culture methods. However, the adoption of these MDx assays has been so quick that in some cases it outpaced evidence of clinical utility. The need for healthcare professional education (e.g., physicians, clinical pharmacy) is also a challenge to consider. Physicians must understand the limitations to and appropriate utilization of these technologies in order to provide cost-effective and well-informed care for their patients.
Routes to become MDx Professionals
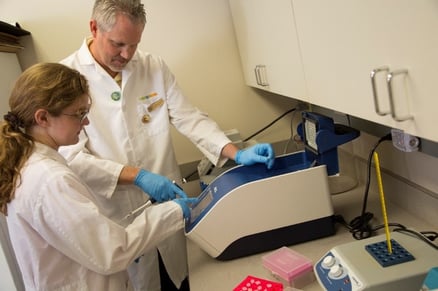
The ability of a medical laboratory professional (or other appropriate laboratory professional) to perform molecular diagnostic testing has become critical to the laboratory medicine profession. Knowledge of methodology associated with detection and surveillance of pathogens, cancer biomarkers, inherited genetic disorders or other biomarkers is imperative for the current and future professional. The field is currently in need of well-trained medical laboratory professionals with strong biomedical science and medical laboratory science backgrounds and a thorough understanding of technologies used in assay development who can bridge the current state of practice with continuing developments in high complexity testing.
The best way to work in the field of MDx, command a handsome salary and learn to validate new molecular assays is to become a certified technologist in molecular biology. The American Society for Clinical Pathology (ASCP) Board of Certification (BOC) offers a certification exam for eligible candidates. A bachelor's or master’s degree from a National Accrediting Agency for Clinical Laboratory Sciences (NAACLS)-accredited Diagnostic Molecular Science (DMS) program or Medical Laboratory Science (MLS) program is the fastest route to become eligible to sit for the exam. There are currently 8 NAACLS-accredited DMS programs offering a variety of options, ranging from certificates to undergraduate and graduate degrees. Although less applicable to those interested in infectious disease, there are also NAACL- accredited program in cytogenetics, and ASCP (BOC) offers a technologist in cytogenetics (CG) certification exam. Currently, there are only 4 NAACLS-accredited programs in the U.S. for cytogenetics. These degrees (DMS and CG) give graduates the skills to immediately start working in the field and validating new molecular assays to expand the molecular testing menu for more personalized patient care.
The issues surrounding the advancement of molecular diagnostics will continue to grow in the race to enhance care for individuals using genomic and metagenomic information. Those in the field need to be adaptable, analytical and ethically responsible to forge a new and exciting path of personalized medicine.
Article adapted from American Society for Microbiology. July 7, 2021


Share Article