
Lessons From COVID Can Help U.S. Advance Health Equity
Former U.S. Surgeon General Jerome Adams, MD, MPH, is passionate about several things. First is his family, i.e., his wife, Lacey, and their three children. Second is public service. (He led the Indiana State Department of Health before serving as the 20th Surgeon General of the United States from 2017-2021.) And third is building communities in which no one faces barriers to the care they need, regardless of zip code, gender, race or income level.
Today Dr. Adams is Distinguished Professor and the Director of Health Equity Initiatives at Purdue University, and he teaches clinical anesthesia at Eskenazi Health in downtown Indianapolis. He also serves as chairman of the Association of Diversity in Clinical Trials.
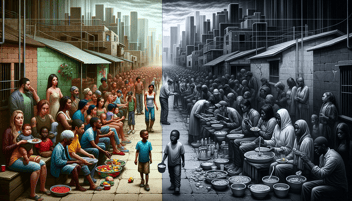
In a recent conversation with executives and Commercial Teams from SEKISUI Diagnostics and Aptitude Medical Systems, Dr. Adams pointed out how the COVID pandemic challenged healthcare providers and public health professionals in the U.S. and across the globe. “But hunger, famine, pandemic and genocide will happen again, and we need to figure out how to go in and help people prosper going forward,” he said.
He offers some ideas in his 2023 book, “Crisis and Chaos: Lessons from the Front Lines of the War Against COVID-19,” and shared some of them with the group, including:
- Improving how health professionals present the potential impact of public health emergencies on people’s everyday lives.
- Maintaining a broad approach in allocating healthcare resources during national emergencies.
- Promoting at-home testing and screening.
- Addressing the “health debt,” particularly on behalf of those who suffer most from it.
Engage in Meaningful Conversations
“My initial focus on being named Surgeon General was on mental health challenges and addressing the opioid epidemic,” he said in his conversation with SEKISUI Diagnostics. But those priorities changed in January 2020, when news of the virus in China made its way across the globe. It wasn’t until March 11, 2020, when the National Basketball Association suspended its season after Utah Jazz center Rudy Gobert tested positive for COVID-19 prior to the beginning of a game against the Oklahoma City Thunder that most of America paid attention.
“Few people paid attention to what health officials were saying until their sports and businesses started to be affected,” said Dr. Adams. “That told us we need to learn to speak to our audience in a way that resonates, not just with health statistics.”
Expanding Perspectives
During the pandemic, “we ignored many mental and physical health threats while focusing on COVID, and we can’t afford to do that again,” he said. “We can’t focus so much on one thing that we ignore others, such as opioid overdoses, cancer screening or preventive care. It doesn’t help to save lives from one threat if you put people’s lives at risk from another.”
During the pandemic, “we ignored many mental and physical health threats while focusing on COVID, and we can’t afford to do that again,”
Revolutionizing Healthcare Access: The Power of At-Home Testing
Dr. Adams believes that the world saw a revolution in point-of-care testing during the pandemic, but especially with at-home testing. “We learned we can make healthcare more accessible to people who can’t take off work for a test or who lack childcare or transportation. And we need to make more testing available not just for infectious diseases, but for non-communicable ones, such as cancer.”
COVID also led healthcare providers to appreciate the benefit of home monitoring. “We talk about white coat hypertension,” he said. “It’s like taking your car to the shop and it won’t make the noise it was making at home. If we can monitor a patient throughout the day or week, then feed that information to the clinician, that clinician can make more informed decisions about care.
“Ultimately, there are many ways for testing and monitoring to improve access and equality of care.”
Addressing the Burden of Healthcare Neglect
Americans need to recognize the “health debt” incurred during the pandemic, that is, the adverse outcomes caused by denial of medical care because of the focus on COVID, he continued. “We have to acknowledge it, and we have to acknowledge it affects some communities more than others. We have to deploy resources to the communities that were hardest hit by that health debt so they can catch up. And we must do the same to address the ‘education debt’ caused by missed school.
“We can point fingers and lament these debts, but we have to figure out how to overcome them.” A good starting point is toning down the rhetoric and finger-pointing so that all can focus on actual solutions.
Dr. Jerome Adams
20th Surgeon General of the United States
Distinguished Professor, Presidential Fellow & Executive Director of Health Equity Initiatives at Purdue



Share Article