All age groups, not just young people need to pay attention, take precautions
The incidence of sexually transmitted infections (STIs) among those ages 55 and over is on the rise. That is cause for concern, as STIs among this age group can lead to other serious illnesses, such as heart disease, cancer and even HIV.1
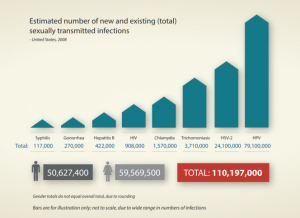
The rise among this age group coincides with a rise in STIs among the general population. Data published in 2021 by the U.S. Centers for Disease Control and Prevention (CDC) show that reported annual cases of sexually transmitted diseases (STDs) in the United States continued to climb in 2019, reaching an all-time high for the sixth consecutive year.2 (Sexually transmitted diseases begin as sexually transmitted infections, or STIs.)
The findings signal a disappointing reversal of what had been a positive trend. “Less than 20 years ago, gonorrhea rates in the U.S. were at historic lows, syphilis was close to elimination, and advances in chlamydia diagnostics made it easier to detect infections,” said Raul Romaguera, DMD, MPH, who was acting director for CDC’s Division of STD Prevention when the data was published. “That progress has since unraveled, and our STD defenses are down.”2
Why is this occurring?
The fact that people in their mid-50s and older contract STIs should come as little surprise, as a substantial proportion of people in this age group are sexually active. According to a 2007 survey of 3,005 adults in the U.S. aged 57–85 years, 83.7%, 67.0%, reported sexual activity with a partner in the previous 12 months. 3
A 2015 study from the University of Manchester in England found that people continue to engage in sexual activity into their 70s and 80s.4 Data from the English Longitudinal Study showed that more than half (54%) of men and almost a third (31%) of women over the age of 70 reported they were still sexually active, with a third of the men and women having sex at least twice a month.
And a study from Sweden published in 1996 found that 46% of men aged 70-80 years reported having at least one orgasm in the previous month.5 A U.S. study from 2007 found that in the previous year, 60% of elderly men and 30% of elderly women had had sexual intercourse.
An at-risk population
Sexually active seniors may be more susceptible to STIs than young people.6 As people age, they stand a greater chance of developing a health condition that weakens the immune system, increasing the risk of contracting an infection. In addition, women lose estrogen due to menopause, and thinning of the vaginal tissues can leave them vulnerable to microabrasions, increasing susceptibility to STIs. And since many people in this age group no longer fear pregnancy, they may neglect condom use.
Lack of knowledge is another risk factor. Older people may be unaware that they can contract an STI through oral and anal sex, as well as vaginal intercourse. Also, while divorce marks the end of sexual activity for some older adults, for others it may be the beginning of dating after a long period of monogamy. Those who haven’t dated in many years may feel uncomfortable talking to their partners or healthcare professionals about safe sex.
Safe sex
Seniors need information about safe sex, just as young people do. A literature review published in 2015 found that only about 20% of men and 24% of women aged 50+ years who were not in a long-term relationship with only one partner reported condom use during their last sexual event.3
The American Geriatrics Society’s Health in Aging Foundation offers four tips on having and enjoying safe sex7:
- Know your partner’s sexual background before having oral, vaginal, or anal sex. Talk about sexual histories, past STIs, results of STI testing, and whether either of you has ever injected illegal drugs. Before having sex, check your partner’s penis or vaginal area for sores, abnormal discharge, or odors.
- Consider getting tested first. The best way to protect yourself and your partner is for the two of you to get tested for HIV and other STIs before you start having sex. A person can have an STI and not know it because the symptoms are not obvious. And some symptoms of STIs or HIV, such as tiredness, can be mistaken for age-related health problems.
- Use a condom and lubricant during vaginal, oral, or anal sex, including during foreplay, until you know your partner’s sexual history, STI status, and are in a sexually exclusive relationship. Using water-based lubricants is important because they can lower the chances of getting a sore or tiny cut on the penis or inside the vagina. These sores and cuts can increase the risk of getting STIs.
- Talk to your healthcare provider. They can offer advice about protecting yourself from STIs and when sex is safe with certain medical conditions, such as after a heart attack. Your provider can also recommend treatments for common sexual problems such as vaginal dryness and erectile dysfunction.
Time to talk
Unfortunately, frank conversations between older people and their physicians about sexual activity can be rare. Barriers to communication about sexuality include intimidation, shame, fear of disrespecting the physician, sociodemographic differences, fear of exposing sexual orientation, and fear of inability or disinterest on the part of the physician.5 Elderly people may be embarrassed to discuss their sex lives because of stereotypical images of the asexual elder. They may fear being perceived as perverted or luxurious for having an active sex life, or that their sexual difficulties will be subject to humor.
But physicians can be barriers to communication as well. They may believe that senior people are not interested in sex; they may perceive the patient as being similar to the physician’s own parent; or they may believe another physician specialist is responsible for dealing with the issue. The physician’s religious and/or sexual issues, or (particularly for male physicians) embarrassment in dealing with the sexuality of older women, can also stifle communication.
For all these reasons, clinicians need to stay informed about sexual risk behaviors in the older age group and preventive interventions specifically designed for them. As older adults often see their primary care doctors at least annually, opportunities to intervene abound. These interventions may include providing written psychoeducational materials, such as the pamphlets targeting diabetes care or hypertension that patients often read while in physicians’ waiting rooms.
Primary care providers should be aware that older individuals – just as their young counterparts -- are more likely to engage in unprotected sex when under the influence of alcohol or recreational drugs. For that reason, providers should inquire about alcohol and drug use in this age group, and specifically about its use preceding or during sexual activity.
Prevention efforts should target men who have sex with men (MSM) separately, as they may not feel comfortable sharing their concerns with older heterosexual adults or with younger MSM. Because the prevalence of HIV infection is high among older MSM, condom use is an essential tool to prevent transmission of the virus from those who are HIV-positive to those who are HIV-negative.
Footnotes
- Historic High Rates Of STIs Among Older Americans, Forbes
- Reported STDs reach all-time high for 6th consecutive year, U.S. Centers for Disease Control and Prevention
- Sexual risk behaviors and HIV risk among Americans aged 50 years or older: a review, Substance Abuse and Rehabilitation
- Love and intimacy in later life: study reveals active sex lives of over-70s, University of Manchester
- Assessment of physicians’ addressing sexuality in elderly patients with chronic pain, Einstein (Sao Paulo)
- https://www.everydayhealth.com/stds/rise-sharply-among-older-americans/
- Tip Sheet for Safe Sex in older adults

Share Article